By Chad Terhune
(Reuters) – Drugs like Wegovy may trim your waistline but not medical costs, according to an analysis of U.S. health insurance claims shared with Reuters.
The full-year cost of care for U.S. patients with obesity two years after starting on Novo Nordisk’s Wegovy or similar GLP-1 drugs was $18,507, on average. That represents a 46% jump over the average annual medical cost of $12,695 prior to taking the medication, data provided by pharmacy benefits manager Prime Therapeutics show.
The costs for a similar control group of patients not taking the drugs grew by 14% for the same period.
Among GLP-1 patients, prescription drug costs drove most of the spending increase, but medical costs also climbed over the two-year period.
Over the two-year period, the analysis found “no reduction in obesity-related medical events,” such as heart attacks, strokes and diagnoses of type 2 diabetes, or use of prescription drugs for hypertension and high cholesterol, compared to the control group.
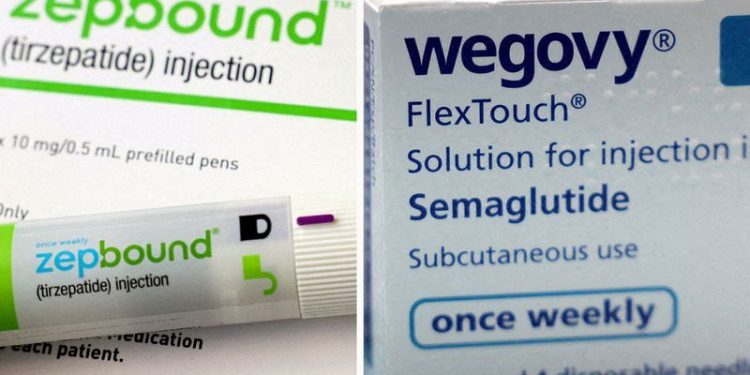
Novo and rival Eli Lilly (NYSE:LLY), which makes the GLP-1 weight-loss drug Zepbound, have reaped billions of dollars in profits since their new drugs hit the U.S. market, with only a fraction of an estimated 100 million patients with obesity having used them.
They say use of their medicines will yield savings for society by alleviating many health problems linked to excess weight.
Yet many U.S. employers and government health officials remain wary of adding coverage for these highly effective, but expensive medicines due to the significant upfront investment and uncertainty about any future savings.
“The budget hit here is frightening for a lot of governments and private entities,” said Ben Ippolito, an economist at the American Enterprise Institute. “What makes these drugs different is the sheer size of the potential demand.”
Some analysts have said the weight-loss drug market could reach $150 billion a year in the next decade.
“We know treatment of obesity is linked to better medical outcomes, even if bureaucrats haven’t figured out how to account for these savings,” Novo Nordisk (NYSE:NVO) said in a statement. Lilly did not respond to a request for comment.
NOT ‘FULLY CONCLUSIVE’
Prime Therapeutics reviewed pharmacy and medical claims data for 3,046 people with commercial health plans that cover GLP-1 drugs. They had all received new GLP-1 prescriptions between January and December 2021, and had a diagnosis of obesity or a body mass index of 30 or higher.
In the analysis, 46% of patients were taking Novo’s Ozempic or Wegovy, both injectable versions of semaglutide. Others were taking older Novo drugs Saxenda or Victoza, which are both liraglutide, Rybelsus, an oral version of semaglutide, or Lilly’s Trulicity (dulaglutide).
The researchers didn’t track long-term use of Lilly’s newer GLP-1 drugs, Mounjaro and Zepbound (both tirzepatide), which launched after the study began.
Prime excluded patients with a diabetes diagnosis in their medical claims or who were using a drug for type 2 diabetes, for which these medicines were originally developed. The mean age of patients in the analysis was 46 and 81% were female.
Patrick Gleason, assistant vice president for health outcomes at Prime and a co-author of the analysis, said employers and insurers should be prepared to spend an additional $11,200 for every patient taking a GLP-1 drug for obesity during the first two years of therapy due to the price and lack of reduction in related medical costs.
The estimate reflects drugmakers’ discounts for these medications but not all rebates, he said.
In this analysis, only one-in-four patients prescribed Wegovy or Ozempic for weight loss were still taking the medications two years later, which Reuters reported in July.
David Lassen, the PBM’s vice president for pharmacy clinical services, said it may be challenging to replicate the health benefits demonstrated in clinical trials because so few patients stick with their prescriptions.
“I don’t think it’s fully conclusive at this point,” Lassen told Reuters, saying three years of data may be necessary to gauge the cost impact.
“We want to do everything possible to help individuals achieve the positive outcomes of being on this medication,” Lassen said. “But if we determine there is not a positive outcome with our data and there is not a return on investment, that will be an inflection point ahead that we will have to consider.”
Prime is owned by 19 U.S. Blue Cross and Blue Shield health insurance plans and manages pharmacy benefits for about 38 million people.
The company estimates that fewer than 20% of members have coverage for weight-loss drugs. Prime said it’s supportive of clients’ decision to cover these GLP-1 drugs in combination with lifestyle modification programs.
Valerie Smith, an associate professor of population health sciences at Duke University, said her research into bariatric surgery also found no reduction in medical costs even when weight loss was maintained for many years.
However, she said this analysis may mask potential savings among specific groups of patients, such as those with severe obesity or multiple chronic conditions.